
Hypertensive Crisis: Do we treat Hypertensive Urgencies?
Nov 15, 2024I had a 68 yo patient recently who was being admitted. Prior to going to the ward, the nurse approached me with news that the patient's blood pressure was 190-200 mmHg systolic. The admission diagnosis was unrelated to this blood pressure. "He can't go to the ward with this blood pressure, as it will activate Medical Emergency Team Criteria. Can you give him something please?" The patient was well and had no signs of end organ damage. Would you treat?
The term 'hypertensive urgency' is a misnomer. It implies that there is an urgent need to treat. Treating asymptomatic hypertensive patients is the exception to, rather than the rule. Intensive treatment of elevated blood pressure without end organ damage has been found to result in harm.
The first thing we need to do is to ensure the right cuff is used, the patient is in the right position and that we address any issues that might be increasing the patient's blood pressure such as pain and anxiety.
It is important to identify those patients with hypertensive emergencies where there is an accelerated rise in blood pressure, causing end organ damage and differentiate them from those patients who have a longstanding poorly controlled blood pressure, but are symptomatic. It is also important to differentiate those patients who have transient elevation in blood pressure due to pain or anxiety.
Historical we may have used the following terms:
- Hypertensive crisis: elevated BP, eg, SBP/DBP >180/110–120 mm Hg, with or without new or worsening target-organ damage) ie., patients with an elevated blood pressure that can be symptomatic or asymptomatic
- Hypertensive Emergency was defined as the elevated blood pressure with new or worsening target organ damage and
- Hypertensive urgency: elevated BP without evidence of new or worsening target-organ damage
We know the importance of treating those patients with end organ damage, however there is less definitive guidance, and no randomised trials for treating those patients who are asymptomatic.
A new Scientific Statement by the American Heart Association on the ‘Management of Elevated Blood Pressure in the Acute Care Setting’ (1), proposes a new approach to patients with elevated blood pressures, based on the presence or absence of symptoms.
In this statement they propose:
- Assymptomatic Patients with:
- elevated BP (SBP/DBP ≥130/80 mm Hg) without evidence of new or worsening target-organ
- markedly elevated BP (SBP/ DBP >180/110–120 mm Hg without evidence of new or worsening target-organ damage), and
- Symptomatic Patients with elevated blood pressures ie., hypertensive emergency (SBP/DBP >180/110–120 mm Hg with evidence of new or worsening target-organ damage),
- It is important to remember that end organ damage can occur at lower blood pressures.
- Examples of end organ damage includes:
- brain (eg, hypertensive encephalopathy, intracranial hemorrhage, and acute ischemic stroke),
- heart (eg, acute myocardial infarction, unstable angina, acute left ventricular failure with pulmonary edema), l
- Large vessels (dissecting aortic aneurysm),
- Kidneys, and the microvasculature manifestations may include conditions such as high-grade retinopathy, acute kidney injury, or microangiopathic hemolytic anemia and thrombocytopenia.
Measuring Blood Pressure
How we measure blood pressure and the context in which it is measured are important. Is the patient in pain? Are they very anxious?
Other factors that play a role are: patient positioning ie., sitting vs lying, where the arm is placed and cuff placement and cuff size.
We know that with very high and very low blood pressures the oscillometric devices are not as accurate. At high blood pressures ie., >180/110, oscillometric devices may underestimate blood pressures by as much as 50/30mmHg when compared to an arterial line (2). In patients with a potential hypertensive emergency, the use of an arterial line is imperative, to get an accurate initial blood pressure reading, but also to monitor the lowering of blood pressure.
Asymptomatic Hypertension
Treating the asymptomatic patient with hypertension, especially if already on antihypertensives, may result in a short term decrease in blood pressure, but may also affect the need for the patient's own blood pressure medication, to later be witheld. No randomized clinical trials have looked at the treatment of asymptomatic hypertensive patients. Observational studies have shown that treatment of asymptomatic hypertension, especially with intravenous agents has been associated with organ injury including, myocardial Injury, acute kidney injury and stroke (4). Treating asymptomatic hypertensive patients is the exception to, rather than the rule.
Hypertensive Emergency
Hypertensive emergencies are usually accelerated, severe elevations in blood pressure, that are associated with target organ injury. There is no definite threshold of blood pressure, although >180/110 mm Hg is used. Most organ injury tends to occur at blood pressures >220/110 mmHg (3)
- Ensure that the correct cuff size and technique is used to take the blood pressure.
- Look for target organ damage; both new and worsening.
- Take a specific history
- Current anti-hypertensive medications and adherence
- Chronic hypertension history
- Previous blood pressure reading.
- Physical Examination
- Look for a pulse difference, by comparing pulses
- Is there a blood pressure difference in the arms
- Cardiac auscultation
- Fundoscopy
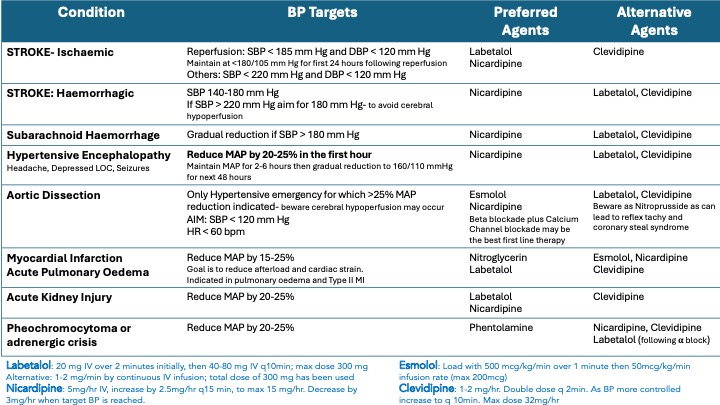
Management of Hypertensive Emergency
Below is a summary table of common presentations and the most appropriate methods to treat.
References
- Bress A P. The Management of Elevated Blood Pressure in the the Acute Care Setting: A Scientific Statement From the American Heart Association. 2024 Aug;81(8):e94 e106
- Ribezzo S, et al. Noninvasive techniques for blood pressure measurement are not a reliable alternative to direct measurement: a randomized crossover trial in ICU. Sci World J. 2014;2014:353628.
- Johnson W, Nguyen M‐L, Patel R. Hypertension crisis in the emergency department. Cardiol Clin 2012;30:533‐
- Anderson TS, Herzig SJ, Jing B, et al. Clinical outcomes of intensive inpatient blood pressure management in hospitalized older adults. JAMA Intern Med 2023;183:715‐
- Miller J.B et al Evaluation and Management of Hypertensive Emergency. BMJ 2024;386:e077205
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Cras sed sapien quam. Sed dapibus est id enim facilisis, at posuere turpis adipiscing. Quisque sit amet dui dui.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.
